- Home
- About Us
- Doctors
- Specialties
- Bariatric Surgery
- Bone Marrow Transplant
- Cancer
- Cardiology
- Cardiovascular And Thoracic Surgery
- Critical Care Medicine
- Dental Surgery
- Dermatology & Cosmetology
- Diabetic Foot Care
- Ear, Nose & Throat
- Endocrinology
- Fetal Medicines
- Gastroenterology
- General Medicine
- General Surgery
- HPB & Gastrointestinal Surgery
- Interventional Radiology
- IVF
- Kidney Transplant
- Laparoscopic Surgery
- Liver Transplant
- Medical And Hemato Oncology
- Neurology
- Neuro & Spine Surgery
- Nephrology And Dialysis
- Nuclear Medicine
- Orthopedic
- Ophthalmology
- Obstetrics And Gynecology
- Pathology Laboratory
- Pediatric
- Peripheral Vascular And Endovascular Surgery
- Physiotherapy and Rehabilitation
- Plastic Reconstruction
- Plastic & Cosmetic Surgery
- Pulmonary Medicine
- Radiation Oncology
- Radiology
- Robotic Surgery
- Surgical Oncology
- Urology
- Facilities
- Patient Area
- Testimonials
- Media
- Contact Us
Gestational Trophoblastic Disease
Placenta of Hope: Uniting for Strength, Inspiring Hope in Pregnancy
Welcome to Universal Hospital’s Gestational Trophoblastic Disease Care, where we are dedicated to providing expert and compassionate care for individuals affected by gestational trophoblastic disease. Gestational trophoblastic disease is a group of rare pregnancy-related tumors that involve abnormal growth of cells in the uterus.
Understanding Gestational Trophoblastic Disease:
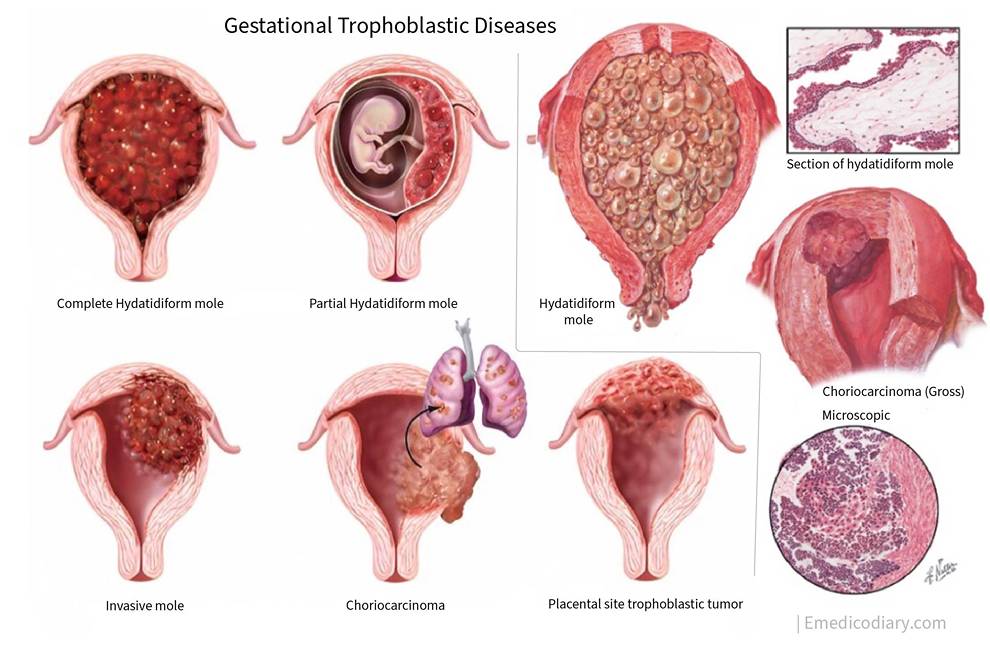
Gestational Trophoblastic Disease (GTD) is a group of rare pregnancy-related tumors that originate from the trophoblast, the tissue that normally surrounds the fertilized egg and helps in the formation of the placenta. GTD includes various conditions, ranging from non-cancerous (benign) to malignant forms. The most common types of GTD are hydatidiform mole, invasive mole, choriocarcinoma, placental-site trophoblastic tumor, and epithelioid trophoblastic tumor.
Types of Gestational Trophoblastic Disease:
- Complete Hydatidiform Mole (CHM): A non-cancerous condition where an abnormal fertilized egg implants in the uterus and forms a mass of cysts.
- Partial Hydatidiform Mole (PHM): Similar to CHM but with a partially formed fetus and abnormal placental tissue.
- Invasive Mole: A type of mole that invades into the uterine wall but is not considered cancer.
- Choriocarcinoma: A malignant and fast-growing cancer that can develop after any type of pregnancy, including normal pregnancies.
- Placental-Site Trophoblastic Tumor (PSTT): A rare but malignant tumor that forms in the uterus at the site where the placenta was attached.
- Epithelioid Trophoblastic Tumor (ETT): Another rare and malignant tumor that typically occurs in reproductive-age women.
Risk Factors:
- Previous Molar Pregnancy: Women who have had a molar pregnancy are at an increased risk.
- Age: GTD is more common in women younger than 20 or older than 35.
- History of Miscarriage or Stillbirth: Previous pregnancy losses may be associated with an increased risk.
- Oral Contraceptive Use: Some studies suggest a reduced risk among women who have used oral contraceptives.
Symptoms:
Symptoms of GTD can vary based on the specific type but may include:
- Vaginal Bleeding: Abnormal bleeding, often more than expected during pregnancy.
- Enlarged Uterus: The uterus may be larger than expected for the gestational age.
- Hyperemesis Gravidarum: Severe nausea and vomiting.
- High Blood Pressure: Hypertension may occur in some cases.
Staging:
Staging for GTD is based on the extent of the disease and the specific type of trophoblastic tumor.
- Hydatidiform Mole (HM):
- A noncancerous (benign) form of GTD characterized by abnormal growth of the placenta.
- Gestational Trophoblastic Neoplasia (GTN):
- GTN includes invasive mole, choriocarcinoma, placental site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor (ETT).
- Stage I:
- The tumor is confined to the uterus.
- Subcategories provide more details, such as whether it involves only the uterus or has spread to blood vessels.
- Stage II:
- The tumor has spread beyond the uterus but is still within the reproductive organs.
- Subcategories provide more details about the extent of spread.
- Stage III:
- The tumor has metastasized to distant organs, such as the lungs.
- Subcategories specify the organs affected.
- Stage IV:
- The tumor has spread to distant sites beyond the reproductive organs and distant metastasis.
- Subcategories provide details about the extent of spread.
Diagnosis:
- Ultrasound: Imaging test to visualize the uterus and the characteristics of the tumor.
- Blood Tests: Measurement of specific hormone levels (hCG) associated with pregnancy and GTD.
- Biopsy: Removal of a tissue sample for laboratory examination to confirm the type of GTD.
Treatment:
- Surgery: Hysterectomy (removal of the uterus) is the primary treatment for early-stage cancer.
- Radiation therapy: Targets and destroys cancer cells.
- Chemotherapy: Systemic treatment to kill cancer cells throughout the body.
Prevention:
Some preventive measures to reduce the risk of endometrial cancer include:
- Maintaining a Healthy Weight: Adopting a healthy diet and lifestyle.
- Hormone Replacement Therapy (HRT): If using HRT, combining estrogen with progesterone may lower the risk.
- Treating Endometrial Hyperplasia: Addressing precancerous conditions promptly.
Prognosis:
- Prognosis depends on the stage at diagnosis, with early-stage cancers having a better outlook.
- Overall survival rates for endometrial cancer are generally favorable.
Screening:
Routine screening for endometrial cancer is not common in the general population. Diagnosis is often prompted by the presence of symptoms or during routine gynecologic examinations.
Why Choose Universal Hospital for Endometrial Cancer Care:
- Expert Gynecologic Oncology Team: Our Endometrial Cancer Care Center is staffed by a team of experienced gynecologic oncologists, surgeons, and supportive care professionals with specialized knowledge in the diagnosis and treatment of endometrial cancer.
- Cutting-Edge Treatments: Universal Hospital offers state-of-the-art treatments, including surgery, radiation therapy, chemotherapy, hormone therapy, and participation in clinical trials, ensuring patients have access to the latest advancements in endometrial cancer care.
- Holistic Patient Care: We prioritize individualized care plans that consider not only the medical aspects of endometrial cancer but also the emotional and practical needs of our patients, providing support and resources beyond the treatment room.





